Understanding the Normal QRS Complex
The normal QRS complex is a critical aspect of cardiac physiology that reflects the electrical activity of the heart during a heartbeat. It plays an essential role in diagnosing various heart conditions. In this article, we will explore what the normal QRS complex is, its components, significance, variations, and the implications of abnormal findings. This comprehensive guide will help you understand the normal QRS complex in detail, making complex cardiac concepts more accessible.
What is the QRS Complex?
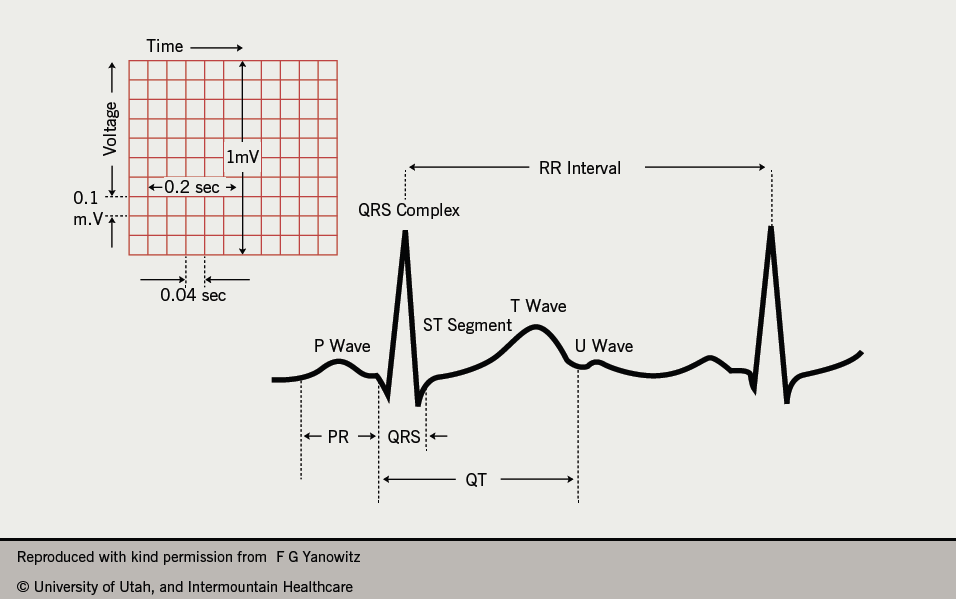
The QRS complex is a part of an electrocardiogram (ECG or EKG), which is a graphical representation of the electrical activity of the heart. The ECG consists of several waves, including the P wave, QRS complex, and T wave. Each part of the ECG waveform corresponds to specific phases of heart activity.
Components of the QRS Complex
- Q Wave: The Q wave is the first downward deflection of the QRS complex. It is often small and represents the initial depolarization of the interventricular septum.
- R Wave: The R wave is the first upward deflection following the Q wave. It is typically the largest component of the QRS complex, indicating the depolarization of the ventricles.
- S Wave: The S wave is the downward deflection that follows the R wave. It represents the final phase of ventricular depolarization.
Duration and Morphology of the Normal QRS Complex
For a QRS complex to be considered normal, it must meet certain criteria:
- Duration: The normal QRS complex duration is between 0.06 and 0.10 seconds (or 60 to 100 milliseconds). A duration longer than this may indicate a delay in the conduction system of the heart.
- Morphology: The normal QRS complex should have a specific shape. It typically appears as a sharp, pointed waveform, with clear distinctions between the Q, R, and S waves. The R wave is generally more prominent than the Q and S waves.
The Significance of the Normal QRS Complex
The normal QRS complex is significant for several reasons:
- Electrical Conduction: The QRS complex represents the rapid depolarization of the ventricles, which is essential for the heart to pump blood effectively. It reflects the heart’s ability to conduct electrical impulses.
- Diagnosis of Heart Conditions: Physicians use the QRS complex to identify various cardiac conditions. Changes in the morphology, duration, or amplitude of the QRS complex can indicate issues such as bundle branch blocks, ventricular hypertrophy, or myocardial infarction.
- Monitoring Heart Health: The normal QRS complex serves as a baseline for assessing heart health. Regular ECGs can help detect any changes in the QRS complex that might indicate developing heart problems.
Variations in the QRS Complex
While the normal QRS complex is critical, variations can occur for several reasons. Some common variations include:
1. Bundle Branch Blocks
Bundle branch blocks occur when there is a delay or obstruction in the electrical conduction system of the heart. This can lead to a wider QRS complex, typically exceeding 0.10 seconds. There are two types of bundle branch blocks:
- Left Bundle Branch Block (LBBB): This occurs when the electrical impulse is delayed in the left bundle branch, leading to a characteristic QRS pattern on the ECG.
- Right Bundle Branch Block (RBBB): In this case, the impulse is delayed in the right bundle branch, resulting in a different QRS morphology.
2. Ventricular Hypertrophy
Ventricular hypertrophy refers to the thickening of the heart muscle, often due to high blood pressure or other cardiac conditions. This can lead to changes in the QRS complex, such as increased amplitude, as the thicker muscle requires more electrical activity to depolarize.
3. Myocardial Infarction
A myocardial infarction (heart attack) can significantly alter the QRS complex. In this case, the depolarization pattern may be disrupted, leading to changes such as the development of pathological Q waves, which can indicate previous heart damage.
The Relationship Between the QRS Complex and Heart Rate
The QRS complex is closely related to heart rate. As heart rate increases, the time between QRS complexes decreases, resulting in a faster rhythm. This is observed in conditions such as tachycardia. Conversely, bradycardia, or a slower heart rate, will result in a longer interval between QRS complexes.
1. Tachycardia
In tachycardia, the heart rate exceeds 100 beats per minute. The QRS complex may remain normal in shape but can become closer together on the ECG. If the tachycardia is due to a re-entrant circuit, the QRS may be narrow; however, if it is due to ventricular tachycardia, the QRS may be wider and more abnormal in morphology.
2. Bradycardia
Bradycardia occurs when the heart rate drops below 60 beats per minute. In this case, the intervals between QRS complexes are longer. In some cases, bradycardia may be normal, such as in athletes, but if it is symptomatic, further investigation is necessary.
Assessing the Normal QRS Complex
To assess the normal QRS complex, healthcare professionals rely on the interpretation of ECG readings. The process includes:
- ECG Recording: An ECG is performed using electrodes placed on the skin. These electrodes detect the electrical activity of the heart and generate a waveform on paper or a digital display.
- Measurement: The duration and morphology of the QRS complex are measured. Healthcare providers look for the following:
- Is the QRS duration within the normal range (0.06 to 0.10 seconds)?
- Are the Q, R, and S waves clearly defined?
- Is the overall shape consistent with a normal QRS complex?
- Analysis: After measurement, the provider will analyze the QRS complex in the context of other waves (like the P wave and T wave) and the overall heart rhythm.
Clinical Implications of Abnormal QRS Complexes
Abnormalities in the QRS complex can indicate various underlying health issues. Here are some conditions associated with an abnormal QRS complex:
1. Arrhythmias
Arrhythmias are irregular heartbeats that can arise from problems with the electrical conduction system. For instance, atrial fibrillation can lead to irregularly timed QRS complexes due to chaotic electrical signals in the atria.
2. Cardiac Ischemia
Cardiac ischemia, which occurs when the heart muscle does not receive enough blood, can lead to changes in the QRS complex. This can manifest as ST-segment changes or T-wave inversions on the ECG, indicating potential heart problems.
3. Electrolyte Imbalances
Electrolyte imbalances, such as high potassium (hyperkalemia) or low magnesium (hypomagnesemia), can also affect the morphology and duration of the QRS complex. For example, hyperkalemia can lead to a wider QRS complex.
Conclusion
Understanding the normal QRS complex is vital for healthcare professionals and anyone interested in heart health. The normal QRS complex not only reflects the electrical activity of the heart but also serves as a key indicator for diagnosing and monitoring various heart conditions.
By recognizing what constitutes a normal QRS complex, its significance, variations, and the implications of abnormalities, we can appreciate the complexity of cardiac health. Regular monitoring through ECGs is essential for maintaining heart health and catching potential issues early on.
This guide serves as an introduction to the normal QRS complex, but further study and practical experience are necessary for a comprehensive understanding of cardiac electrophysiology and its clinical implications.