The heart is a remarkable organ that plays a crucial role in our overall health. One of the vital aspects of heart health that medical professionals monitor is the PR interval. In this article, we will explore the concept of the normal PR interval, its significance, how it’s measured, and what deviations from the norm might mean for your health.
What is the PR Interval?
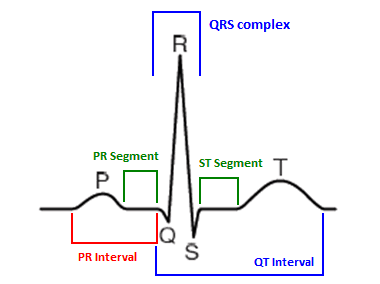
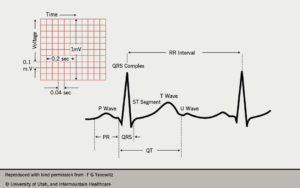
The PR interval is a segment of the electrocardiogram (ECG or EKG) that represents the time it takes for electrical impulses to travel from the atria (the upper chambers of the heart) to the ventricles (the lower chambers). It is measured from the beginning of the P wave, which represents atrial depolarization, to the beginning of the QRS complex, which signifies ventricular depolarization.
Components of the ECG
To understand the PR interval fully, it’s essential to know a bit about the components of the ECG:
- P Wave: This wave represents the depolarization of the atria. It indicates that the atria are contracting and pushing blood into the ventricles.
- QRS Complex: This series of waves represents the depolarization of the ventricles. It is typically larger and sharper than the P wave because the ventricles are more muscular than the atria.
- T Wave: This wave represents the repolarization of the ventricles, indicating that the ventricles are getting ready for the next heartbeat.
Importance of the PR Interval
The PR interval is an essential marker for assessing heart function. It provides insights into the conduction system of the heart, particularly regarding how well electrical signals are transmitted between the atria and ventricles. A normal PR interval typically ranges from 120 to 200 milliseconds (ms).
Abnormalities in the PR interval can indicate underlying conditions. A PR interval that is too short or too long may suggest issues with the heart’s electrical system, which could lead to various cardiac disorders.
Measuring the Normal PR Interval
The Electrocardiogram (ECG) Procedure
To measure the PR interval, an ECG is performed. This procedure involves placing electrodes on the skin, which detect the electrical activity of the heart and produce a graphical representation of this activity. The steps involved in an ECG procedure include:
- Preparation: The patient is asked to lie down comfortably, and the skin where the electrodes will be placed is cleaned to ensure good conductivity.
- Electrode Placement: Small sticky patches (electrodes) are placed on the chest, arms, and legs. These electrodes are connected to an ECG machine.
- Recording: The patient is usually asked to remain still and breathe normally while the machine records the heart’s electrical activity for a few seconds.
- Analysis: Once the recording is complete, healthcare professionals analyze the ECG strip to measure the PR interval and other components.
Interpreting the Results
To determine the normal PR interval, healthcare providers look at the distance between the P wave and the beginning of the QRS complex on the ECG strip. This measurement is typically expressed in milliseconds. A normal PR interval ranges from 120 to 200 ms:
- Less than 120 ms: A shorter PR interval may indicate conditions such as Wolff-Parkinson-White syndrome, where there is an extra electrical pathway in the heart.
- Greater than 200 ms: A longer PR interval may indicate first-degree atrioventricular (AV) block, which occurs when electrical signals are delayed as they pass through the AV node.
Factors Influencing the PR Interval
The normal PR interval can be influenced by various factors, including:
Age
As individuals age, the conduction system of the heart can change, potentially leading to variations in the PR interval.
Heart Rate
The heart rate can also affect the PR interval. A faster heart rate can sometimes lead to a shorter PR interval.
Medications
Certain medications, especially those that affect the heart’s electrical activity (like beta-blockers), can alter the PR interval.
Electrolyte Imbalances
Imbalances in electrolytes, such as potassium and calcium, can affect heart function and the PR interval.
Clinical Significance of PR Interval Abnormalities
Short PR Interval
A short PR interval (less than 120 ms) can be indicative of several conditions:
- Wolff-Parkinson-White Syndrome: This condition is characterized by an extra electrical pathway in the heart, which can lead to rapid heartbeats (tachycardia).
- Atrial Fibrillation: In some cases, a short PR interval may be associated with atrial fibrillation, where the heart’s upper chambers beat chaotically and irregularly.
Long PR Interval
A long PR interval (greater than 200 ms) can signify several conditions, including:
- First-Degree AV Block: This is the most common type of AV block, characterized by a delay in the conduction through the AV node. While it usually does not cause symptoms or require treatment, it may indicate a higher risk of developing more severe forms of heart block.
- Second-Degree AV Block: This condition can be further classified into two types (Type I and Type II). It involves intermittent failures of conduction from the atria to the ventricles, and it may require monitoring or treatment depending on severity.
- Medication Effects: Certain medications, like digoxin or beta-blockers, can prolong the PR interval.
Symptoms Related to PR Interval Abnormalities
In many cases, individuals with PR interval abnormalities may not experience noticeable symptoms. However, some potential symptoms associated with significant PR interval changes may include:
- Palpitations: An awareness of the heartbeat, often felt as a racing or irregular pulse.
- Dizziness or Lightheadedness: This can occur if the heart is not pumping effectively.
- Fatigue: General tiredness may occur, particularly if the heart is not functioning efficiently.
- Fainting: In severe cases, significant conduction delays can lead to fainting spells (syncope).
Diagnostic Procedures Beyond ECG
While an ECG is the primary method for assessing the PR interval, other diagnostic tools may be used to provide additional information:
Holter Monitor
A Holter monitor is a portable ECG device that continuously records the heart’s activity for 24 to 48 hours. This can help identify intermittent changes in the PR interval that may not be captured during a standard ECG.
Event Monitor
Similar to a Holter monitor, an event monitor records heart activity but is activated by the patient when they experience symptoms. This can be useful in diagnosing transient abnormalities in the PR interval.
Electrophysiology Study (EPS)
In some cases, healthcare providers may recommend an electrophysiology study. This invasive procedure involves threading catheters through the blood vessels to the heart to assess its electrical system in detail.
Treatment Options for PR Interval Abnormalities
Treatment for PR interval abnormalities depends on the underlying cause and the severity of the condition.
Monitoring
In cases of first-degree AV block, no specific treatment is usually necessary, and the condition may simply be monitored over time.
Medications
For patients with significant symptoms or those diagnosed with conditions like Wolff-Parkinson-White syndrome, medications may be prescribed to manage heart rhythm.
Pacemaker Insertion
In cases of more severe AV blocks (like second-degree or third-degree AV block), a pacemaker may be necessary. A pacemaker is a small device implanted under the skin that helps regulate the heart’s electrical activity, ensuring it beats at a proper rate.
Lifestyle Modifications for Heart Health
To support overall heart health and potentially improve the PR interval, consider the following lifestyle modifications:
Diet
A heart-healthy diet is essential. Focus on:
- Fruits and Vegetables: Aim for a variety of colorful fruits and vegetables to ensure a wide range of nutrients.
- Whole Grains: Foods like brown rice, quinoa, and whole wheat bread can help maintain healthy blood pressure and cholesterol levels.
- Lean Proteins: Opt for sources like fish, poultry, beans, and legumes.
- Healthy Fats: Include sources of omega-3 fatty acids, such as fish, flaxseeds, and walnuts.
Regular Exercise
Engaging in regular physical activity can strengthen the heart, improve circulation, and help maintain a healthy weight. Aim for at least 150 minutes of moderate-intensity aerobic activity each week.
Stress Management
Chronic stress can negatively impact heart health. Techniques such as mindfulness, meditation, yoga, and deep breathing exercises can be beneficial.
Avoid Smoking and Limit Alcohol
Smoking is a significant risk factor for heart disease. Quitting smoking can greatly improve heart health. Additionally, if you consume alcohol, do so in moderation.
Regular Check-Ups and Monitoring
Regular check-ups with a healthcare provider are essential for maintaining heart health, especially if you have risk factors for heart disease or a history of heart-related issues. Your provider can monitor your PR interval and other vital signs, providing early intervention if needed.
Conclusion
The normal PR interval is an essential aspect of heart health, reflecting the efficiency of electrical conduction in the heart. Understanding what constitutes a normal PR interval and the implications of deviations can help individuals and healthcare providers work together to maintain optimal heart function. Regular monitoring and proactive management of heart health through lifestyle changes and medical interventions can significantly impact overall well-being.
As we continue to learn more about heart health, recognizing the importance of the PR interval is crucial in the early detection and treatment of potential heart-related issues. If you have concerns about your heart health or have experienced symptoms related to PR interval abnormalities, don’t hesitate to consult a healthcare professional.