Understanding ST Elevation ECG: A Comprehensive Guide
Electrocardiograms (ECGs) are vital tools used in medicine to assess the heart’s electrical activity. Among the various findings that can be observed on an ECG, one of the most significant is ST elevation, which can indicate serious cardiac conditions. This article will explore the ST elevation ECG, detailing its causes, significance, diagnosis, and treatment. Our goal is to provide a thorough understanding of this critical topic.
What is an ST Elevation ECG?
An ST elevation ECG is characterized by an upward deflection in the ST segment of the ECG waveform. This deviation is measured relative to the baseline and can suggest acute myocardial infarction (heart attack), pericarditis, or other conditions affecting the heart. The ST segment represents the period between ventricular depolarization and repolarization, and any significant deviation from the norm can be clinically relevant.
The Importance of ST Segment Analysis
Analyzing the ST segment is crucial for diagnosing various cardiac conditions. The ST segment normally remains flat (isoelectric) during rest and shows minimal variation in healthy individuals. An elevation of more than 1 mm (0.1 mV) above the baseline in two or more contiguous leads is considered significant and can lead to the suspicion of myocardial injury or other cardiac issues.
Common Causes of ST Elevation
There are several conditions that can cause ST elevation on an ECG. Understanding these causes is essential for accurate diagnosis and treatment. Some of the most common include:
- Acute Myocardial Infarction (AMI): This is the most critical condition associated with ST elevation. In the case of an ST-Elevation Myocardial Infarction (STEMI), the heart muscle is severely damaged due to a blocked coronary artery, leading to characteristic ST segment changes.
- Pericarditis: Inflammation of the pericardium (the membrane surrounding the heart) can lead to ST elevation. Unlike STEMI, the ST elevation in pericarditis is usually concave and often involves multiple leads.
- Early Repolarization: This is a benign condition often seen in younger individuals, characterized by ST elevation, primarily in the precordial leads.
- Brugada Syndrome: A genetic condition that can cause life-threatening arrhythmias. The ST elevation in this syndrome occurs in specific leads and is associated with a high risk of sudden cardiac death.
- Ventricular Aneurysm: After a myocardial infarction, scar tissue can form in the heart, leading to a ventricular aneurysm, which can also cause ST elevation.
- Hyperkalemia: Elevated potassium levels in the blood can affect the heart’s electrical activity, resulting in ST segment changes, including elevation.
Recognizing ST Elevation on ECG
To understand ST elevation ECG better, it’s essential to know how to identify it. Healthcare professionals use specific criteria to determine ST elevation. The most accepted criteria include:
- Elevation in the ST Segment: Measured at the J-point (where the QRS complex ends and the ST segment begins).
- Contiguous Leads: Elevation must be present in at least two contiguous leads (leads that are anatomically or functionally related).
- Amplitude: The elevation is typically considered significant if it exceeds 1 mm in limb leads or 2 mm in precordial leads.
Interpreting the ECG
To effectively interpret an ST elevation ECG, it is vital to evaluate the entire ECG, not just the ST segment. The following components should be analyzed:
- P Wave: Represents atrial depolarization. Changes can indicate atrial enlargement or other conditions.
- QRS Complex: Indicates ventricular depolarization. Widened QRS complexes can suggest a bundle branch block or other conduction abnormalities.
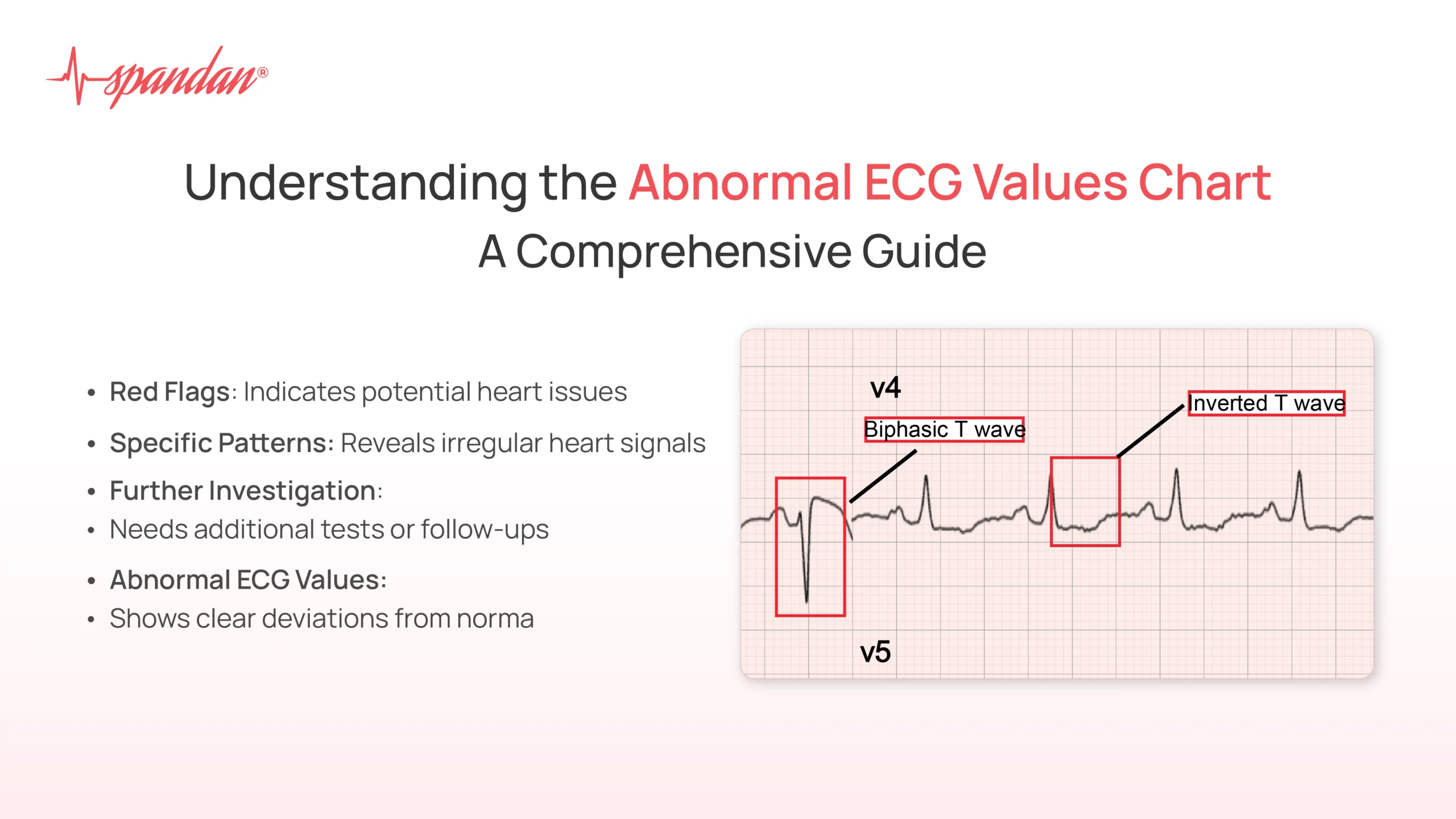
- T Wave: Represents ventricular repolarization. T wave inversion or flattening can accompany ST elevation, indicating myocardial ischemia.
Clinical Significance of ST Elevation ECG
ST elevation has significant clinical implications, particularly in emergency medicine. When ST elevation is detected, it often prompts immediate action due to its association with life-threatening conditions.
ST-Elevation Myocardial Infarction (STEMI)
The most critical condition linked to ST elevation is STEMI. It is essential for healthcare providers to recognize this condition quickly because timely intervention can save lives. Here’s a detailed look at STEMI:
- Pathophysiology: STEMI occurs due to the rupture of an atherosclerotic plaque, leading to the formation of a thrombus (blood clot) that obstructs a coronary artery. This blockage prevents oxygen-rich blood from reaching part of the heart muscle, resulting in ischemia and eventual necrosis (cell death).
- Symptoms: Common symptoms of STEMI include chest pain (often described as a pressure or squeezing sensation), shortness of breath, nausea, sweating, and pain that radiates to the arm, jaw, or back.
- Diagnosis: An ECG is the primary diagnostic tool for STEMI. In addition to ST elevation, other findings such as new Q waves or T wave inversions may be present. Blood tests for cardiac biomarkers, such as troponin, are also performed to confirm the diagnosis.
- Treatment: Immediate treatment for STEMI includes restoring blood flow to the affected coronary artery. This can be achieved through medication (thrombolytics) or procedures such as percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG).
The Diagnostic Process
When a patient presents with symptoms suggestive of cardiac issues, a systematic approach is essential. The diagnostic process typically includes:
- History and Physical Examination: Gathering a detailed medical history and performing a physical exam to identify risk factors and symptoms.
- ECG Acquisition: A 12-lead ECG is typically performed to assess the heart’s electrical activity. The presence of ST elevation in the appropriate leads can indicate a need for immediate intervention.
- Cardiac Biomarkers: Blood tests to check levels of cardiac enzymes (like troponin) can help confirm myocardial injury.
- Imaging Studies: Additional imaging studies such as echocardiograms or cardiac MRI may be conducted to evaluate the heart’s structure and function.
Management and Treatment
The management of ST elevation on an ECG is primarily focused on addressing the underlying cause. Here’s a breakdown of the treatment options based on the identified condition:
Acute Myocardial Infarction
- Immediate Care: Patients with ST elevation indicating a STEMI require urgent care, often in an emergency department. The goal is to restore blood flow as quickly as possible.
- Medications: Patients may receive aspirin to thin the blood, beta-blockers to reduce heart workload, and statins to lower cholesterol levels.
- Interventional Procedures: If indicated, procedures like angioplasty and stent placement are performed to open blocked arteries.
Pericarditis
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) are often the first line of treatment for inflammation. In severe cases, corticosteroids may be prescribed.
- Monitoring: Patients may need regular follow-ups to monitor the condition and prevent complications such as cardiac tamponade.
Early Repolarization
- Reassurance: In most cases, early repolarization is a benign finding, requiring no specific treatment. However, patients should be educated about the condition.
Brugada Syndrome
- Management: Patients may require an implantable cardioverter-defibrillator (ICD) if they are at high risk for arrhythmias.
Hyperkalemia
- Treatment: Addressing the underlying cause of hyperkalemia is crucial. Treatments may include medications to lower potassium levels and dietary modifications.
Monitoring and Follow-Up
After initial treatment for conditions associated with ST elevation, ongoing monitoring is crucial. This may include:
- Regular ECGs: To track changes in the heart’s electrical activity.
- Cardiac Rehabilitation: A structured program to help patients recover after a heart event, focusing on physical activity, nutrition, and education.
- Follow-Up Appointments: Regular visits to a healthcare provider to monitor heart health and manage risk factors.
Conclusion
Understanding ST elevation ECG is vital for healthcare providers and anyone interested in cardiac health. Recognizing the significance of ST elevation can lead to early diagnosis and treatment of potentially life-threatening conditions, particularly acute myocardial infarction. By learning to interpret ECGs and understanding the underlying causes of ST elevation, patients and providers can work together to promote heart health and prevent serious complications.