Understanding PAC EKG: A Comprehensive Guide
Electrocardiograms (EKGs) are vital tools used in medicine to assess the heart’s electrical activity. Among the various types of EKG patterns, the term “PAC EKG” refers to the EKG readings associated with premature atrial contractions (PACs). In this article, we will delve into what PAC EKG means, how to recognize it, its causes, symptoms, diagnosis, and treatment options. By the end of this comprehensive guide, you will have a clearer understanding of PAC EKG and its significance in cardiac health.
What Are Premature Atrial Contractions (PACs)?
Before diving into PAC EKG, it’s essential to understand what PACs are. PACs are early heartbeats that originate in the atria, the upper chambers of the heart. These contractions occur before the regular heartbeat and can disrupt the normal rhythm of the heart. While they are often benign, PACs can sometimes be a sign of underlying heart conditions.
Key Characteristics of PACs
- Early Contraction: PACs occur before the expected heartbeat, leading to an irregular rhythm.
- Atrial Origin: These contractions originate in the atria rather than the ventricles.
- Symptoms: Most individuals with PACs experience no symptoms, although some may feel palpitations or a skipped beat.
The Importance of PAC EKG
Understanding PAC EKG is crucial for identifying these early contractions on an EKG reading. Recognizing PACs through EKG can help healthcare providers determine the appropriate course of action and treatment options, if necessary.
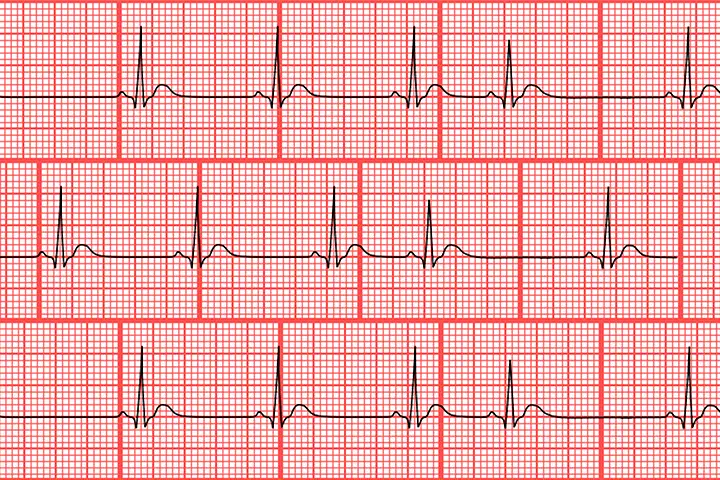
The Anatomy of an EKG
To comprehend PAC EKG, one must first understand the basic components of an EKG. An electrocardiogram displays the electrical activity of the heart in the form of waves. Here are the essential elements of an EKG:
- P Wave: Represents atrial depolarization or the contraction of the atria.
- QRS Complex: Represents ventricular depolarization or the contraction of the ventricles.
- T Wave: Represents ventricular repolarization or the recovery phase of the ventricles.
How PAC EKG Looks
In a PAC EKG, the most notable feature is an early P wave, which can look different from the normal P waves. Here’s what you might see:
- Early P Wave: The PAC occurs earlier than expected, leading to an early P wave on the EKG.
- Normal QRS Complex: After the early P wave, the QRS complex typically remains normal unless there are other underlying issues.
Causes of PACs
Understanding the causes of PACs is essential for managing the condition effectively. PACs can arise from various factors, including:
1. Stimulants
- Caffeine: Excessive caffeine intake can lead to PACs. It’s found in coffee, tea, energy drinks, and soft drinks.
- Nicotine: Smoking or using tobacco products can trigger PACs due to its stimulant effects on the heart.
2. Stress and Anxiety
Emotional stress and anxiety can lead to increased adrenaline levels, which may cause PACs.
3. Electrolyte Imbalances
Imbalances in electrolytes, such as potassium, magnesium, and calcium, can disrupt the heart’s electrical system, leading to PACs.
4. Heart Disease
Although PACs are often benign, they can occur more frequently in individuals with underlying heart conditions, such as:
- Coronary artery disease
- Heart valve disorders
- Hypertension
5. Alcohol Consumption
Heavy drinking or binge drinking can lead to PACs, especially in individuals who may not regularly consume alcohol.
6. Medications
Certain medications, especially those that stimulate the heart, may lead to PACs as a side effect.
Symptoms of PACs
Most individuals with PACs do not experience noticeable symptoms. However, some may report the following:
- Palpitations: A feeling of the heart fluttering or racing.
- Skipped Beats: A sensation that the heart skipped a beat or had an irregular rhythm.
- Dizziness: Occasionally, some people may feel lightheaded, especially if PACs are frequent.
If you experience frequent or concerning symptoms, it’s essential to consult a healthcare provider for further evaluation.
Diagnosing PACs
When diagnosing PACs, healthcare providers may utilize various methods, including:
1. Patient History
The healthcare provider will take a thorough medical history, including any symptoms, lifestyle factors, and family history of heart disease.
2. Physical Examination
A physical exam may include checking your pulse and listening to your heart. Abnormal heart rhythms can often be detected during this examination.
3. Electrocardiogram (EKG)
An EKG is the primary diagnostic tool for identifying PACs. The healthcare provider will analyze the EKG for:
- Early P Waves: Indicating the presence of PACs.
- QRS Complex: Assessing whether the QRS complex remains normal.
4. Holter Monitor
If PACs are not detected during a standard EKG, a healthcare provider may recommend a Holter monitor, which is a portable EKG device worn for 24 to 48 hours to continuously monitor the heart’s activity.
5. Event Monitor
Similar to a Holter monitor, an event monitor is used for longer periods (weeks to months) and can be activated by the patient when they experience symptoms.
Treatment Options for PACs
In many cases, PACs are benign and do not require treatment. However, if PACs are frequent or symptomatic, various treatment options may be considered.
1. Lifestyle Changes
- Avoid Stimulants: Reducing or eliminating caffeine and nicotine can help decrease the frequency of PACs.
- Stress Management: Practicing relaxation techniques, such as yoga, meditation, or deep breathing exercises, can help manage stress and reduce PAC occurrences.
- Regular Exercise: Engaging in regular physical activity can promote overall heart health.
2. Medications
If PACs are symptomatic or linked to underlying heart conditions, healthcare providers may prescribe medications, including:
- Beta-blockers: These medications can help regulate heart rate and rhythm.
- Anti-arrhythmic drugs: Used to help restore a normal heart rhythm.
3. Catheter Ablation
In rare cases, when PACs are frequent and cause significant symptoms, a healthcare provider may recommend catheter ablation. This procedure involves inserting a catheter into the heart to destroy the small area of heart tissue that is causing the PACs.
4. Monitoring and Follow-Up
For individuals with infrequent or asymptomatic PACs, regular monitoring and follow-up appointments may be sufficient. This allows healthcare providers to keep track of any changes in the heart’s rhythm and adjust treatment plans accordingly.
Living with PACs
Living with PACs can be concerning, especially for those experiencing symptoms. Here are some tips for managing the condition:
1. Stay Informed
Educating yourself about PACs and their implications can help reduce anxiety. Understanding what to expect and when to seek medical attention is essential.
2. Maintain a Healthy Lifestyle
Incorporating heart-healthy habits, such as a balanced diet, regular exercise, and avoiding harmful substances, can help manage PACs and improve overall heart health.
3. Communicate with Healthcare Providers
Regular check-ups and open communication with healthcare providers can help address any concerns and ensure that any changes in symptoms are monitored appropriately.
4. Support Groups
Joining support groups or forums can provide a sense of community and help individuals share their experiences with others facing similar challenges.
Conclusion
PAC EKG is an important aspect of understanding premature atrial contractions and their implications for heart health. While PACs are often benign, recognizing their presence on an EKG can lead to proper evaluation and management. By understanding the causes, symptoms, diagnosis, and treatment options associated with PACs, individuals can take proactive steps to maintain their cardiovascular health. Always consult with a healthcare provider if you have concerns about your heart rhythm or experience any unusual symptoms.
Final Thoughts
Remember, PACs are common and often not a cause for alarm. However, staying informed and being proactive about your heart health can help you lead a healthier life. Whether you experience PACs occasionally or frequently, understanding their impact through PAC EKG will empower you to make informed decisions regarding your health.