Understanding Junctional Escape Rhythm: Insights into Cardiac Function
Junctional escape rhythm is a fascinating aspect of cardiac physiology that plays a crucial role in the heart’s electrical system. To understand this rhythm, it is essential to explore its mechanisms, clinical significance, and implications for patient care. In addition, the Basic Principle of Biosafety emphasizes the need for safety when working with biological systems, which includes a thorough understanding of cardiac function. This article aims to provide an in-depth examination of junctional escape rhythm, exploring its characteristics, causes, diagnosis, treatment, and the relevance of biosafety principles in medical practice.
What is Junctional Escape Rhythm?
Junctional escape rhythm is a type of cardiac rhythm that originates in the atrioventricular (AV) junction, which is the area of tissue between the atria and the ventricles. This rhythm serves as a backup mechanism for the heart, ensuring that it continues to beat even when the normal pacemaker (the sinoatrial node, or SA node) fails to function properly.
Characteristics of Junctional Escape Rhythm
- Rate: Junctional escape rhythms typically have a heart rate ranging from 40 to 60 beats per minute. This is slower than the normal resting heart rate, which usually ranges from 60 to 100 beats per minute.
- Rhythm: The rhythm is usually regular, but it can occasionally be irregular depending on the underlying causes.
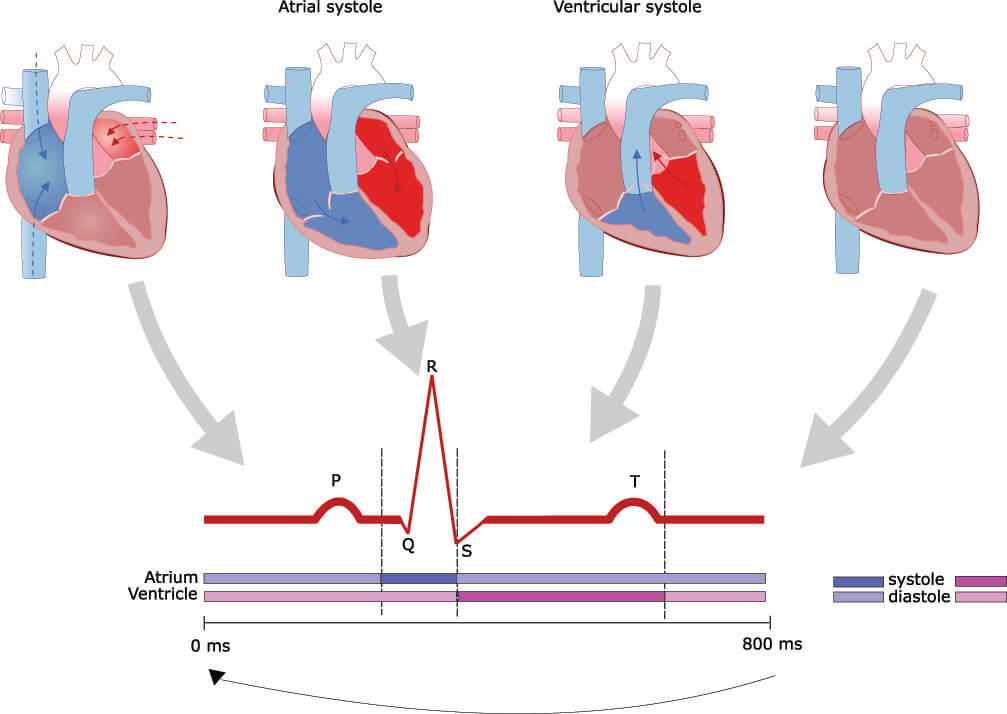
- P Waves: In junctional escape rhythm, P waves (which represent atrial depolarization) may be absent, inverted, or occur after the QRS complexes (which represent ventricular depolarization). This is a key characteristic that distinguishes it from other rhythms.
- QRS Complex: The QRS complex is typically narrow, indicating that the ventricles are depolarizing normally.
Function of Junctional Escape Rhythm
The primary function of the junctional escape rhythm is to maintain a viable heart rate in the event of SA node failure. The AV junction can take over as the pacemaker under these circumstances, ensuring that the heart continues to pump blood effectively.
Causes of Junctional Escape Rhythm
Understanding the underlying causes of junctional escape rhythm is essential for appropriate diagnosis and treatment. Several factors can lead to this rhythm, including:
1. SA Node Dysfunction
The most common cause of junctional escape rhythm is dysfunction of the SA node. This can occur due to various reasons, including:
- Ischemia: Reduced blood flow to the SA node can impair its function, leading to junctional escape rhythms.
- Inflammation: Conditions such as myocarditis can cause inflammation of the heart muscle, affecting the SA node’s ability to generate impulses.
2. AV Node Blockage
If there is a complete heart block (third-degree AV block), the SA node may be unable to communicate with the ventricles. In such cases, the AV junction can take over as a pacemaker, resulting in a junctional escape rhythm.
3. Medication Effects
Certain medications, particularly those that affect heart rate and conduction, can lead to junctional escape rhythms. Examples include:
- Beta-Blockers: These drugs decrease heart rate and can impair SA node function.
- Calcium Channel Blockers: These medications can also reduce heart rate and conduction through the AV node.
4. Electrolyte Imbalances
Electrolyte disturbances, particularly involving potassium and calcium, can affect the heart’s electrical system. Low potassium levels (hypokalemia) or high potassium levels (hyperkalemia) can lead to junctional escape rhythms.
5. Cardiac Structural Abnormalities
Structural changes in the heart, such as cardiomyopathy or fibrosis, can disrupt normal electrical conduction pathways, leading to junctional escape rhythms.
Clinical Significance of Junctional Escape Rhythm
Recognizing junctional escape rhythm is critical for healthcare providers, as it can be indicative of underlying cardiac issues.
Symptoms
Patients with junctional escape rhythm may exhibit various symptoms, including:
- Fatigue: A slower heart rate can result in decreased cardiac output, leading to fatigue.
- Dizziness or Lightheadedness: Reduced blood flow to the brain may cause dizziness or fainting episodes.
- Palpitations: Patients may feel their heart beating irregularly or slower than usual.
Diagnosis
The diagnosis of junctional escape rhythm typically involves several steps:
- Electrocardiogram (ECG): An ECG is the primary tool used to identify junctional escape rhythm. The characteristic features, such as absent or inverted P waves and a regular QRS complex, are evaluated.
- Patient History: A thorough patient history is essential to identify any underlying conditions or medications that may contribute to the rhythm.
- Physical Examination: A physical exam can help assess for symptoms and any potential underlying causes.
Treatment
The treatment of junctional escape rhythm focuses on addressing the underlying cause. Potential management strategies include:
- Adjusting Medications: If medications are responsible for the rhythm, healthcare providers may modify dosages or switch to alternative treatments.
- Electrolyte Replacement: In cases of electrolyte imbalances, appropriate supplementation can help restore normal rhythm.
- Pacemaker Placement: In severe cases, particularly those involving complete heart block, a pacemaker may be necessary to ensure adequate heart function.
Junctional Escape Rhythm and the Basic Principle of Biosafety
Understanding the relationship between cardiac rhythms and biosafety is crucial, especially in healthcare settings. The Basic Principle of Biosafety emphasizes protecting patients, healthcare workers, and the environment from potential hazards. Here’s how it relates to junctional escape rhythm:
Safe Handling of Patients with Cardiac Issues
When managing patients with junctional escape rhythm, healthcare providers must ensure:
- Proper Monitoring: Continuous ECG monitoring can help detect any changes in the rhythm and provide timely intervention.
- Infection Control: Practicing strict infection control measures is essential, especially if invasive procedures such as pacemaker insertion are required.
Education and Training
Healthcare professionals must receive proper education and training on:
- Recognizing Junctional Escape Rhythm: Training can enhance early identification and appropriate management of this rhythm.
- Understanding Biosafety Protocols: Familiarity with biosafety principles ensures a safe environment for both patients and staff.
Prognosis and Outcomes
The prognosis for patients with junctional escape rhythm largely depends on the underlying cause. If the rhythm is a temporary response to a reversible condition, such as medication effects or electrolyte imbalance, patients may recover fully with appropriate management.
Long-term Management
For patients with persistent junctional escape rhythms due to structural heart disease or complete heart block, ongoing management may include:
- Regular Follow-up: Continuous monitoring and follow-up appointments are essential to track heart health.
- Lifestyle Modifications: Encouraging heart-healthy lifestyle changes, such as diet and exercise, can improve overall cardiac function.
Patient Education
Educating patients about their condition, potential symptoms, and when to seek medical help is crucial for promoting better health outcomes. Patients should be informed about:
- Recognizing Symptoms: Knowing the warning signs of worsening heart function can lead to timely intervention.
- Importance of Medication Adherence: Taking prescribed medications as directed is essential for maintaining heart rhythm stability.
Conclusion
Junctional escape rhythm is a critical aspect of cardiac physiology that demonstrates the heart’s remarkable ability to adapt in the face of challenges. Understanding this rhythm’s characteristics, causes, clinical significance, and treatment options is essential for effective patient care. Moreover, integrating the Basic Principle of Biosafety into cardiac care practices ensures that patients and healthcare workers remain safe during diagnosis and treatment.
By fostering a thorough understanding of junctional escape rhythm, healthcare professionals can provide better care, enhance patient outcomes, and contribute to a safer healthcare environment. As ongoing research continues to expand our knowledge of cardiac rhythms, the importance of education and training in biosafety remains paramount in ensuring the health and safety of all individuals involved in the care process.
This article provides an overview of junctional escape rhythm, but further research and continuous education are vital for those involved in the field of cardiology and patient care. Understanding the complexities of cardiac rhythms and their implications can significantly impact patient health and safety.