Understanding ECG Lead Placement: A Simple Guide
Electrocardiograms, commonly known as ECGs or EKGs, are essential tools used by doctors to monitor and evaluate the heart’s electrical activity. This guide will help you understand what ECG lead placement is, why it matters, and how it’s done. Whether you’re a healthcare professional or just curious about heart health, this article will simplify the topic so everyone can grasp the key points, even a five-year-old!
What is ECG Lead Placement?
ECG lead placement refers to the specific locations on the body where electrodes are attached to record the heart’s electrical signals. Think of electrodes as tiny listeners that pick up signals from your heart, helping doctors see how it’s working. Proper placement of these leads is crucial because it ensures that the readings are accurate. Imagine trying to listen to music, but the speakers are placed too far away or in the wrong direction; you wouldn’t hear the song clearly!
When you go to a hospital or clinic, a healthcare provider will often place these electrodes on your chest, arms, and legs. The electrodes connect to a machine that records the heart’s activity, creating a picture called an electrocardiogram. This picture helps doctors identify problems such as irregular heartbeats or other heart issues.
Why is ECG Lead Placement Important?
Correct ECG lead placement is vital for several reasons:
- Accuracy of Results: Just like a camera needs to be focused to take a clear picture, electrodes need to be placed correctly to get accurate heart readings. Misplaced leads can result in false readings, leading to incorrect diagnoses.
- Identifying Heart Problems: Doctors use the ECG to identify various heart conditions. Proper lead placement allows them to see how well the heart is functioning and if there are any issues, such as blockages or irregular rhythms.
- Monitoring Patient Health: ECGs are used to monitor patients during surgery, in intensive care units, or when they have heart conditions. Correct lead placement ensures continuous and accurate monitoring.
- Guiding Treatment Decisions: The information gathered from an ECG can help guide treatment decisions. If the ECG shows problems, doctors can choose the best course of action to help the patient.
In short, good ECG lead placement is essential for understanding how the heart is doing and making sure patients receive the right care.
Types of ECG Leads
There are two main types of ECG leads: limb leads and precordial leads.
Limb Leads
Limb leads are placed on the arms and legs. They help create a basic view of the heart’s electrical activity. There are usually three limb leads, labeled I, II, and III. Each lead looks at the heart from a different angle, like a team of friends watching a movie from different seats in the theater.
- Lead I: This lead measures the electrical activity between the right arm and the left arm.
- Lead II: This lead measures the activity from the right arm to the left leg. It’s often the most commonly used lead because it shows the heart’s rhythm clearly.
- Lead III: This one measures the electrical activity from the left arm to the left leg.
Precordial Leads
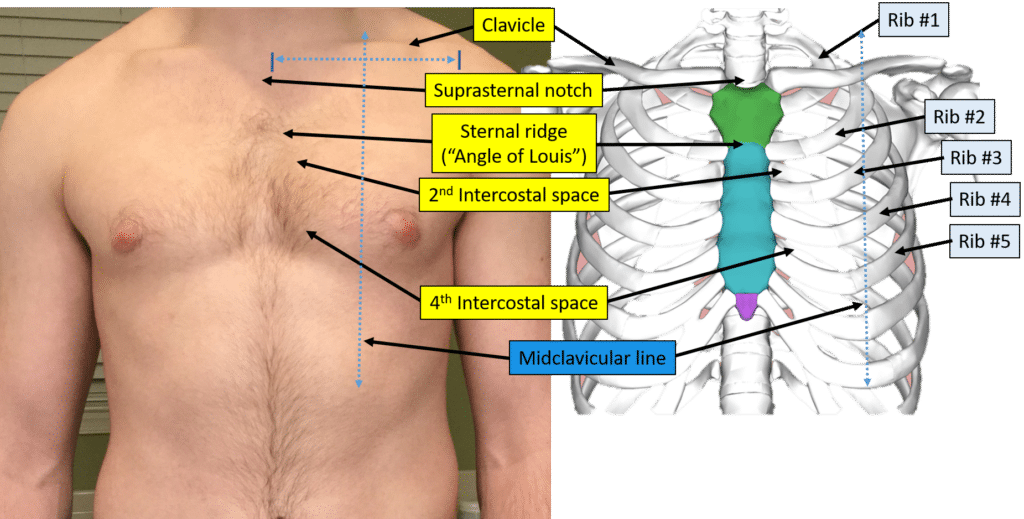
Precordial leads are placed on the chest. These leads provide a closer look at the heart’s electrical activity and are labeled V1 to V6. They help doctors see specific areas of the heart in detail.
- Lead V1: Placed in the fourth intercostal space to the right of the sternum.
- Lead V2: Placed in the fourth intercostal space to the left of the sternum.
- Lead V3: Placed between leads V2 and V4.
- Lead V4: Placed in the fifth intercostal space at the midclavicular line.
- Lead V5: Placed at the same horizontal level as V4, but at the anterior axillary line.
- Lead V6: Placed at the same level as V4 and V5, but at the midaxillary line.
Understanding these lead placements helps us appreciate how doctors can see different parts of the heart and identify any problems.
How to Place ECG Leads
Placing ECG leads correctly is a crucial step that healthcare providers follow to ensure accurate readings. Here’s a step-by-step guide to ECG lead placement.
Step 1: Gather Equipment
Before starting, the healthcare provider gathers all necessary equipment, including:
- ECG machine
- Electrodes (leads)
- Alcohol swabs to clean the skin
- Gel or adhesive for better electrode contact
Step 2: Prepare the Patient
The patient may need to lie down comfortably. The healthcare provider explains the procedure to make the patient feel relaxed. It’s essential to ensure that the skin is clean and free from oils or lotions that could affect the electrode’s ability to pick up signals.
Step 3: Clean the Skin
Using alcohol swabs, the provider cleans the areas where the electrodes will be placed. This step is important because it removes dirt and oils, helping the electrodes stick better and ensuring clear readings.
Step 4: Place the Limb Leads
The provider first places the limb leads on the patient’s arms and legs. Here’s how:
- Right Arm: Place the electrode on the inner aspect of the right arm, just above the wrist.
- Left Arm: Place the electrode on the inner aspect of the left arm, just above the wrist.
- Right Leg: Place the electrode on the inner aspect of the right leg, just above the ankle.
- Left Leg: Place the electrode on the inner aspect of the left leg, just above the ankle.
Step 5: Place the Precordial Leads
After placing the limb leads, the provider proceeds to place the precordial leads:
- Lead V1: Place in the fourth intercostal space to the right of the sternum.
- Lead V2: Place in the fourth intercostal space to the left of the sternum.
- Lead V3: Place between leads V2 and V4.
- Lead V4: Place in the fifth intercostal space at the midclavicular line.
- Lead V5: Place at the same horizontal level as V4 but at the anterior axillary line.
- Lead V6: Place at the same level as V4 and V5 but at the midaxillary line.
Step 6: Check Connections
Once all leads are in place, the healthcare provider checks to ensure that each electrode has good contact with the skin and that all connections to the ECG machine are secure. If any lead seems loose, adjustments will be made to ensure a proper connection.
Step 7: Start the ECG
With everything in place, the provider starts the ECG machine, which begins recording the heart’s electrical signals. The patient may need to remain still during this process to avoid artifacts on the ECG reading.
Common Mistakes in ECG Lead Placement
Even experienced healthcare providers can make mistakes during ECG lead placement. Here are some common errors to avoid:
- Misplacement of Leads: Placing the electrodes in the wrong location can lead to inaccurate readings. Always follow the standardized placement guidelines.
- Poor Skin Preparation: Not cleaning the skin well can cause the electrodes to not adhere properly, leading to poor contact and artifacts in the reading.
- Movement During the Test: If the patient moves while the ECG is being recorded, it can create noise on the graph. Patients should be advised to remain still and calm.
- Not Checking Connections: Forgetting to check the connections can lead to missing data or interruptions in the readings. Always confirm that each lead is connected securely.
- Ignoring Patient Comfort: It’s essential to ensure the patient is comfortable. If a patient is anxious or in pain, it can affect their heart rate and, consequently, the ECG results.
By being aware of these common mistakes, healthcare providers can ensure that they obtain the most accurate and useful information from an ECG.
Understanding the ECG Graph
After the ECG machine records the heart’s electrical signals, it produces a graph. This graph displays various waves, which represent different phases of the heart’s activity. Understanding these waves can help us learn more about heart health.
The P Wave
The P wave represents the electrical activity of the atria, which are the upper chambers of the heart. When the atria contract and pump blood into the ventricles, this wave appears on the ECG graph. A normal P wave indicates that the atria are functioning correctly.
The QRS Complex
The QRS complex shows the electrical activity of the ventricles, the heart’s lower chambers. This part of the graph is usually larger than the P wave because the ventricles are bigger and have to generate more electrical energy to pump blood. A normal QRS complex indicates that the ventricles are contracting properly.
The T Wave
The T wave reflects the recovery phase of the ventricles after they contract. It shows the heart’s readiness to start the next heartbeat. A normal T wave indicates that the heart is recovering well after each contraction.
Arrhythmias and Abnormalities
If the ECG shows irregularities in these waves, it may indicate potential heart problems. For example, a long QRS complex may suggest a delay in the heart’s electrical conduction. Doctors use these patterns to diagnose issues such as arrhythmias or other heart conditions.
Conclusion
In summary, understanding ECG lead placement is crucial for accurate heart monitoring and evaluation. By knowing where to place electrodes, healthcare providers can obtain clear and reliable readings, helping doctors diagnose and treat heart problems effectively. Proper ECG lead placement, along with an understanding of the resulting graphs, plays a vital role in patient care.