Understanding Accelerated Idioventricular Rhythm: A Comprehensive Overview
Accelerated Idioventricular Rhythm (AIVR) is a fascinating and important topic in the field of cardiology. It is a type of arrhythmia, a condition where the heart beats irregularly. Understanding AIVR is crucial for healthcare professionals, patients, and anyone interested in cardiovascular health. This article will explore AIVR in detail, covering its definition, causes, symptoms, diagnosis, treatment options, and more. By the end of this article, you will have a well-rounded understanding of Accelerated Idioventricular Rhythm.
What is Accelerated Idioventricular Rhythm?
Accelerated Idioventricular Rhythm is a specific kind of heart rhythm that originates in the ventricles of the heart. The term “idioventricular” indicates that the rhythm is driven by the ventricles rather than the atria (the upper chambers of the heart). The “accelerated” aspect of the term refers to a heart rate that is faster than the normal rate seen in idioventricular rhythms but slower than that of typical supraventricular tachycardia.
Characteristics of AIVR
AIVR typically has the following characteristics:
- Heart Rate: The heart rate in AIVR usually ranges from 50 to 100 beats per minute. This is higher than the normal idioventricular rate (20-40 beats per minute) but lower than other forms of tachycardia.
- Rhythm Origin: As mentioned, AIVR originates from the ventricles. This means that the electrical impulses that cause the heart to beat come from the ventricular myocardium rather than the usual pacemaker in the atria.
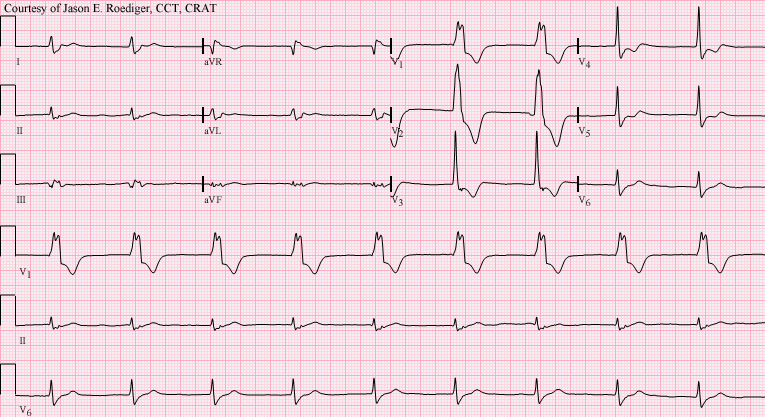
- QRS Complex: The QRS complexes in AIVR tend to be wide and unusual in morphology due to the ventricular origin of the rhythm.
Historical Context
AIVR has been recognized since the mid-20th century, particularly in patients with heart disease. Its clinical significance has evolved, with more recent studies suggesting that it may not always indicate a severe underlying issue. In fact, AIVR can sometimes be a benign finding, especially in specific patient populations.
Causes of Accelerated Idioventricular Rhythm
Several factors can lead to the development of AIVR. Understanding these causes can help in identifying patients who may be at risk. Some of the common causes include:
1. Myocardial Ischemia
Myocardial ischemia occurs when blood flow to the heart muscle is reduced, leading to a lack of oxygen. This condition can trigger AIVR as the heart attempts to compensate for decreased oxygen levels by increasing its rhythm.
2. Acute Myocardial Infarction
In cases of acute myocardial infarction (heart attack), the heart may experience electrical disturbances. AIVR can arise as a result of damage to the heart tissue and altered electrical pathways during and after an infarction.
3. Digoxin Toxicity
Digoxin is a medication used to treat heart conditions. However, when taken in excess, it can lead to toxicity, which may precipitate AIVR. Recognizing and managing digoxin toxicity is vital in preventing AIVR.
4. Electrolyte Imbalances
Electrolytes like potassium and magnesium play crucial roles in heart function. Imbalances in these electrolytes, often caused by dehydration or kidney issues, can lead to AIVR.
5. Cardiomyopathy
Cardiomyopathy is a disease of the heart muscle that can lead to heart failure. Different types of cardiomyopathy can alter the heart’s electrical system, potentially resulting in AIVR.
6. Increased Autonomic Tone
In some cases, increased vagal tone or stimulation of the autonomic nervous system can lead to AIVR. This is often seen in athletes or individuals experiencing stress or anxiety.
7. Post-Cardiac Surgery
AIVR can occur as a complication following cardiac surgery. The heart’s electrical system may be temporarily disrupted during surgery, leading to abnormal rhythms.
Symptoms of Accelerated Idioventricular Rhythm
AIVR may not always produce noticeable symptoms. However, when symptoms do occur, they can vary in severity and presentation. Some common symptoms include:
1. Palpitations
Many patients report feeling a rapid or fluttering heartbeat. These palpitations can be alarming but are often benign.
2. Dizziness or Lightheadedness
Due to the irregular heart rate, some individuals may experience dizziness or a feeling of faintness, particularly if the heart rate becomes excessively fast or slow.
3. Fatigue
An increased heart rate can lead to fatigue, as the heart may struggle to pump effectively during episodes of AIVR.
4. Chest Pain
In cases where AIVR is associated with underlying heart disease, patients may experience chest pain or discomfort. It is crucial to differentiate this from angina or other serious cardiac conditions.
5. Shortness of Breath
Individuals with AIVR may experience difficulty breathing, especially during physical activity or exertion.
6. Syncope
In rare instances, AIVR can lead to fainting (syncope), particularly if blood flow to the brain is compromised.
Diagnosis of Accelerated Idioventricular Rhythm
Diagnosing AIVR typically involves several steps. Healthcare professionals use a combination of medical history, physical examination, and diagnostic tests to arrive at a diagnosis.
1. Medical History
The physician will begin by taking a detailed medical history. This includes information about the patient’s symptoms, any history of heart disease, medications, and lifestyle factors.
2. Physical Examination
A physical exam will be conducted to assess the patient’s overall health and check for signs of heart disease. Vital signs, including heart rate and blood pressure, will be monitored.
3. Electrocardiogram (ECG or EKG)
The most critical test for diagnosing AIVR is an electrocardiogram. An ECG records the electrical activity of the heart and can identify the characteristic wide QRS complexes associated with AIVR.
4. Holter Monitor
In some cases, a Holter monitor (a portable ECG device) may be used to record the heart’s activity over 24-48 hours. This can help capture episodes of AIVR that may not occur during a standard ECG.
5. Echocardiogram
An echocardiogram may be performed to evaluate the structure and function of the heart. This test uses sound waves to create images of the heart and can help identify any underlying conditions contributing to AIVR.
6. Blood Tests
Blood tests may be ordered to check for electrolyte imbalances, kidney function, and any signs of myocardial injury.
Treatment Options for Accelerated Idioventricular Rhythm
Treatment for AIVR depends on the underlying cause, the severity of symptoms, and the patient’s overall health. Here are some common treatment strategies:
1. Observation
In many cases, particularly when AIVR is asymptomatic and not associated with significant underlying heart disease, careful observation may be all that is necessary. Regular follow-ups and monitoring can ensure that any changes are promptly addressed.
2. Medication Management
If AIVR is caused by medications (such as digoxin) or electrolyte imbalances, adjusting dosages or replacing lost electrolytes may resolve the arrhythmia.
3. Antiarrhythmic Medications
In symptomatic cases or when AIVR is persistent, antiarrhythmic medications may be prescribed. These medications help stabilize the heart’s electrical system and reduce the frequency of abnormal rhythms.
4. Cardioversion
In certain situations where AIVR is causing significant symptoms or complications, electrical cardioversion may be necessary. This procedure involves delivering a controlled electrical shock to restore a normal rhythm.
5. Management of Underlying Conditions
Treating the underlying cause of AIVR, such as myocardial ischemia or cardiomyopathy, is essential for long-term management. This may involve lifestyle changes, medications, or interventions like angioplasty or surgery.
6. Lifestyle Modifications
Patients are often advised to make lifestyle changes that can improve heart health and reduce the risk of arrhythmias. These may include:
- Dietary Changes: A heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can promote cardiovascular health.
- Regular Exercise: Engaging in regular physical activity can help improve heart function and reduce the risk of arrhythmias. It is essential to consult with a healthcare provider before starting a new exercise regimen.
- Stress Management: Managing stress through relaxation techniques, mindfulness, or therapy can positively impact heart health.
- Avoiding Stimulants: Reducing the intake of caffeine, nicotine, and other stimulants may help prevent episodes of AIVR.
Prognosis and Outlook
The prognosis for patients with AIVR can vary significantly depending on the underlying cause and individual circumstances. In many cases, AIVR is a transient and benign arrhythmia that resolves with proper management. However, if AIVR is associated with significant heart disease or other serious conditions, the prognosis may be less favorable.
1. Benign Cases
For many individuals, especially those without significant underlying heart disease, AIVR may not pose a serious threat and can be effectively managed through observation and lifestyle modifications.
2. Serious Cases
Conversely, patients with AIVR stemming from myocardial infarction or severe cardiomyopathy may face more complex challenges. These individuals often require ongoing monitoring and comprehensive management strategies.
3. Importance of Follow-Up
Regular follow-up with a healthcare provider is vital for anyone diagnosed with AIV