Fascicular Hemiblock: Understanding Its Implications and Management
Introduction
Fascicular hemiblock is a term used to describe a specific type of heart block that affects the conduction pathways of the heart. It is crucial to understand this condition as it can lead to various cardiac complications if not diagnosed and managed properly. In this article, we will explore the anatomy of the heart, the mechanism of fascicular hemiblock, its causes, symptoms, diagnosis, treatment options, and the long-term outlook for individuals with this condition. By the end of this article, you will have a comprehensive understanding of fascicular hemiblock and its significance in cardiovascular health.
Anatomy of the Heart
To comprehend fascicular hemiblock, it is essential to have a basic understanding of the heart’s anatomy and its electrical conduction system.
The Heart’s Structure
The heart is a muscular organ located in the thoracic cavity, responsible for pumping blood throughout the body. It consists of four chambers: the right atrium, the right ventricle, the left atrium, and the left ventricle. The heart has a network of valves that ensure the unidirectional flow of blood:
- Atrioventricular Valves: These include the tricuspid valve (right side) and the mitral valve (left side), which prevent backflow from the ventricles to the atria.
- Semilunar Valves: The pulmonary valve (right side) and the aortic valve (left side) prevent backflow from the arteries into the ventricles.
Electrical Conduction System
The heart’s ability to pump blood efficiently is governed by its electrical conduction system, which controls the heartbeat. Key components include:
- Sinoatrial (SA) Node: Often referred to as the heart’s natural pacemaker, the SA node initiates electrical impulses that cause the heart to contract.
- Atrioventricular (AV) Node: This node acts as a gatekeeper, controlling the impulses that travel from the atria to the ventricles.
- Bundle of His: This bundle conducts impulses from the AV node into the ventricles through the right and left bundle branches.
- Purkinje Fibers: These fibers distribute the electrical impulse throughout the ventricles, prompting them to contract.
The Role of Fascicles
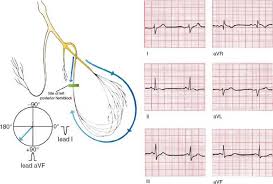
The left bundle branch of the conduction system divides into two fascicles:
- Left Anterior Fascicle
- Left Posterior Fascicle
A fascicular hemiblock occurs when one of these fascicles is blocked, impairing the heart’s electrical conduction.
What is Fascicular Hemiblock?
Fascicular hemiblock refers to the interruption of electrical conduction in one of the two fascicles of the left bundle branch. This condition leads to a delay or block in the transmission of impulses to the heart’s ventricles, resulting in altered heart rhythms. There are two main types of fascicular hemiblock:
- Left Anterior Hemiblock (LAHB)
- Left Posterior Hemiblock (LPHB)
Left Anterior Hemiblock (LAHB)
In LAHB, there is a block in the left anterior fascicle, which causes the electrical impulse to be delayed when it travels to the left ventricle. This can result in changes to the heart’s electrical patterns seen on an electrocardiogram (ECG).
Left Posterior Hemiblock (LPHB)
In LPHB, the block occurs in the left posterior fascicle. Similar to LAHB, this condition also affects the conduction to the left ventricle but has different implications for the heart’s overall electrical activity.
Causes of Fascicular Hemiblock
Fascicular hemiblock can arise from various underlying conditions. Understanding these causes is essential for effective diagnosis and management.
Coronary Artery Disease
Coronary artery disease (CAD) is one of the leading causes of fascicular hemiblock. This condition results from the buildup of plaque in the coronary arteries, which supply blood to the heart muscle. Reduced blood flow can damage the heart’s electrical conduction system, leading to fascicular hemiblock.
Hypertension
High blood pressure can lead to changes in the heart’s structure and function over time. The left ventricle may become hypertrophied (enlarged), which can impact the conduction pathways and contribute to fascicular hemiblock.
Myocardial Infarction
A heart attack can damage the heart muscle and its electrical conduction system. When blood flow is blocked to a portion of the heart, it can lead to ischemia and necrosis, which may result in fascicular hemiblock.
Structural Heart Diseases
Certain congenital or acquired structural heart diseases can predispose individuals to fascicular hemiblock. These conditions may alter the anatomy of the heart and impact electrical conduction.
Other Factors
- Age: Older adults are at a higher risk of developing fascicular hemiblock due to the natural degeneration of the heart’s conduction system.
- Diabetes: Diabetes can damage blood vessels and nerves, contributing to cardiovascular complications, including fascicular hemiblock.
- Electrolyte Imbalances: Imbalances in potassium, calcium, and magnesium can disrupt the heart’s electrical activity, leading to fascicular hemiblock.
Symptoms of Fascicular Hemiblock
Fascicular hemiblock may present with a variety of symptoms, although some individuals may be asymptomatic. Recognizing these symptoms is important for timely diagnosis.
Common Symptoms
- Palpitations: A sensation of a racing or irregular heartbeat.
- Dizziness or Lightheadedness: Reduced blood flow to the brain can cause feelings of faintness.
- Shortness of Breath: Difficulty breathing, especially during physical activity, can occur due to impaired heart function.
- Fatigue: Chronic tiredness may result from the heart’s inability to pump efficiently.
Severe Symptoms
In some cases, fascicular hemiblock can lead to more severe symptoms, such as:
- Chest Pain: This can occur if the heart is not receiving enough oxygenated blood.
- Syncope: Sudden loss of consciousness due to inadequate blood flow to the brain.
It is essential to consult a healthcare provider if any of these symptoms arise, especially if they are severe or recurrent.
Diagnosing Fascicular Hemiblock
Accurate diagnosis of fascicular hemiblock is crucial for effective management. Several diagnostic tools can help identify the condition.
Electrocardiogram (ECG)
An electrocardiogram is the primary tool used to diagnose fascicular hemiblock. The ECG may show characteristic patterns associated with LAHB or LPHB:
- Left Anterior Hemiblock (LAHB): Characterized by left axis deviation, a prolonged QRS complex, and other specific changes.
- Left Posterior Hemiblock (LPHB): Typically associated with right axis deviation and similar QRS changes.
Echocardiogram
An echocardiogram uses sound waves to create images of the heart. This test can help assess the heart’s structure and function, revealing any underlying issues that may contribute to fascicular hemiblock.
Stress Testing
In some cases, a stress test may be conducted to assess how the heart performs under physical stress. This can help identify functional abnormalities that may not be apparent at rest.
Holter Monitor
A Holter monitor is a portable ECG device that continuously records the heart’s electrical activity for 24 to 48 hours. This can help capture any intermittent episodes of fascicular hemiblock.
Treatment Options for Fascicular Hemiblock
The treatment of fascicular hemiblock depends on the underlying cause, severity of symptoms, and overall cardiovascular health.
Lifestyle Modifications
For individuals with mild fascicular hemiblock, lifestyle changes may be sufficient:
- Diet: A heart-healthy diet low in saturated fats, cholesterol, and sodium can help manage risk factors.
- Exercise: Regular physical activity can improve cardiovascular health.
- Smoking Cessation: Quitting smoking significantly reduces the risk of cardiovascular diseases.
- Weight Management: Maintaining a healthy weight is crucial for overall heart health.
Medications
In some cases, medications may be prescribed to manage underlying conditions:
- Antihypertensives: These medications help control blood pressure, reducing strain on the heart.
- Antiplatelet Agents: Drugs like aspirin can help prevent blood clots in individuals with coronary artery disease.
- Statins: These medications can lower cholesterol levels, improving overall heart health.
Advanced Treatments
For individuals with more severe fascicular hemiblock, additional treatments may be necessary:
- Pacemaker: A pacemaker may be implanted to help regulate the heart’s rhythm, especially if the block leads to significant bradycardia (slow heart rate).
- Cardiac Resynchronization Therapy (CRT): In patients with heart failure and fascicular hemiblock, CRT may be considered to improve the heart’s pumping efficiency.
Long-Term Outlook for Individuals with Fascicular Hemiblock
The long-term outlook for individuals with fascicular hemiblock varies based on several factors, including the underlying cause, severity of the condition, and response to treatment.
Prognosis
- Mild Cases: Many individuals with mild fascicular hemiblock may lead normal, active lives with appropriate lifestyle modifications and monitoring.
- Severe Cases: Those with significant underlying heart disease may face a higher risk of complications, including heart failure and arrhythmias.
Importance of Monitoring
Regular follow-up with a healthcare provider is essential for individuals diagnosed with fascicular hemiblock. Routine check-ups, ECG monitoring, and lifestyle assessments can help manage the condition effectively.
When to Seek Medical Attention
Individuals should seek medical attention if they experience worsening symptoms, such as:
- Increased frequency or severity of palpitations.
- Persistent dizziness or lightheadedness.
- New-onset chest pain