Transcutaneous pacing is a vital emergency medical procedure used to manage patients experiencing severe bradycardia, which is an abnormally slow heart rate. This technique involves the use of external electrodes to deliver electrical impulses to the heart, effectively stimulating it to beat at a normal rate. In this article, we will explore the concept of transcutaneous pacing in detail, discussing its mechanisms, indications, procedure, and complications, as well as its role in the broader context of emergency cardiac care.
Understanding Transcutaneous Pacing
Transcutaneous pacing (TCP) is a non-invasive method of cardiac pacing that provides temporary electrical stimulation to the heart. It is often employed in emergency situations when a patient’s heart rate drops dangerously low, leading to symptoms such as dizziness, fainting, or even cardiac arrest. The goal of TCP is to restore an adequate heart rate and improve blood flow to vital organs until more permanent solutions, like transvenous pacing or medication, can be implemented.
How Transcutaneous Pacing Works
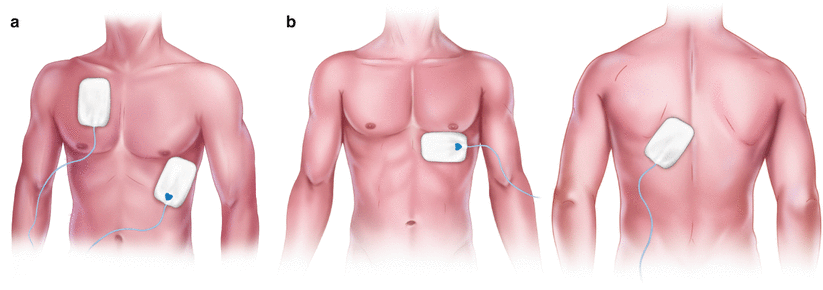
TCP works by delivering electrical impulses through the skin and into the underlying tissues, including the heart muscle. This is achieved using electrodes placed on the chest wall, typically in the anterior-posterior position. The electrical impulses cause depolarization of the heart muscle cells, triggering contraction and thereby increasing the heart rate.
- Electrical Impulses: The pacing device generates electrical impulses at a set rate, usually between 60 and 80 beats per minute, which is typically sufficient for most patients.
- Electrodes Placement: The electrodes are usually placed on the patient’s chest, with one electrode positioned on the anterior chest wall and the other on the back. This placement allows for effective transmission of the electrical current through the heart.
- Output Adjustments: The output of the pacing device can be adjusted based on the patient’s response and the threshold at which the heart muscle contracts effectively.
Indications for Transcutaneous Pacing
Transcutaneous pacing is indicated in various clinical scenarios, primarily involving bradycardia that leads to hemodynamic instability. Some common indications include:
1. Symptomatic Bradycardia
Patients experiencing significant symptoms due to a slow heart rate, such as:
- Dizziness or lightheadedness
- Fatigue
- Shortness of breath
- Chest pain
- Syncope (loss of consciousness)
2. Cardiac Arrest
In cases of pulseless electrical activity (PEA) or severe bradycardia during cardiac arrest, TCP can provide a temporary means of stimulating the heart while resuscitative efforts continue.
3. Drug Overdose
Certain medications, like beta-blockers and calcium channel blockers, can lead to bradycardia. In these cases, TCP may be used until the effects of the drug wear off or until more definitive treatments can be administered.
4. Post-Myocardial Infarction
Bradycardia may occur following a heart attack. TCP can be utilized to maintain cardiac output in these patients while they are stabilized.
Procedure for Transcutaneous Pacing
The procedure for transcutaneous pacing is relatively straightforward, but it requires trained personnel and appropriate monitoring to ensure patient safety and effectiveness.
Step 1: Patient Assessment
Before initiating transcutaneous pacing, it is crucial to assess the patient’s condition:
- Vital Signs: Monitor heart rate, blood pressure, respiratory rate, and oxygen saturation.
- Symptoms: Evaluate the presence of symptoms related to bradycardia.
- Medical History: Take note of any relevant medical history, including medications and previous cardiac conditions.
Step 2: Equipment Preparation
The following equipment is necessary for transcutaneous pacing:
- Pacing Device: An external cardiac pacemaker capable of delivering transcutaneous electrical stimulation.
- Electrodes: Adhesive pads that will be placed on the patient’s chest.
- Monitoring Equipment: A cardiac monitor to observe the patient’s heart rhythm and vital signs during the procedure.
Step 3: Electrode Placement
Proper electrode placement is vital for effective pacing:
- Prepare the Skin: Clean the skin where the electrodes will be placed to ensure good contact.
- Position the Electrodes: Place one electrode on the anterior chest wall (over the right precordial area) and the other on the back, in line with the first electrode.
Step 4: Initiating Pacing
Once the electrodes are in place, the following steps are taken:
- Turn on the Pacing Device: Activate the pacing device and set it to a rate of 60-80 beats per minute.
- Increase Output: Gradually increase the output until capture is achieved, which means the heart responds to the electrical impulses with a contraction.
- Monitor Patient Response: Continuously observe the patient for improvement in symptoms and vital signs. Adjust the pacing output as necessary to maintain effective pacing.
Step 5: Continuous Monitoring
During transcutaneous pacing, it is essential to monitor the following:
- Heart Rhythm: Continuously assess the heart rhythm to ensure effective pacing.
- Patient Comfort: Patients may experience discomfort from the electrical stimulation; adjusting the output or administering sedatives may be necessary.
- Vital Signs: Regularly check blood pressure, heart rate, and oxygen saturation to evaluate the patient’s stability.
Advantages of Transcutaneous Pacing
Transcutaneous pacing offers several benefits in emergency situations:
1. Non-Invasive Procedure
One of the most significant advantages of TCP is that it is non-invasive. Unlike transvenous pacing, TCP does not require catheter placement, reducing the risk of complications.
2. Quick and Easy to Perform
TCP can be rapidly initiated in emergency settings, allowing for prompt treatment of bradycardia and other related cardiac emergencies.
3. Portable Equipment
Most pacing devices are portable, enabling their use in various settings, including ambulances, emergency departments, and even at the patient’s bedside.
4. Temporary Solution
Transcutaneous pacing serves as a temporary measure, providing critical support while more definitive treatments are arranged.
Complications and Considerations
While transcutaneous pacing is generally safe, there are potential complications and considerations to be aware of:
1. Patient Discomfort
The electrical impulses used in TCP can cause discomfort or pain. Patients may require sedation or analgesia to manage this discomfort effectively. For more related articles, visit Healthline Media.
2. Skin Irritation
Prolonged contact with the electrodes may cause skin irritation or burns. Regular monitoring of the electrode sites is essential to prevent skin damage.
3. Ineffective Pacing
In some cases, TCP may not achieve effective capture due to inadequate electrode placement, insufficient output, or patient movement. Continuous monitoring is necessary to ensure effectiveness.
4. Underlying Cardiac Conditions
Patients with significant underlying cardiac issues may require more invasive pacing methods, such as transvenous pacing, if TCP is ineffective.
The Role of Transcutaneous Pacing in Emergency Cardiac Care
Transcutaneous pacing is an essential component of emergency cardiac care. It plays a crucial role in managing patients with bradycardia and is part of the broader strategy to stabilize patients experiencing acute cardiac events. By providing rapid and effective temporary pacing, TCP can significantly improve patient outcomes and facilitate further treatment.
Integration with Advanced Cardiac Life Support (ACLS)
Transcutaneous pacing is often used in conjunction with other advanced cardiac life support (ACLS) interventions. ACLS protocols include various treatments, such as:
- Medications: Administering atropine, epinephrine, or dopamine to manage bradycardia and support cardiac function.
- Defibrillation: If a patient is in cardiac arrest due to ventricular fibrillation or pulseless ventricular tachycardia, immediate defibrillation is prioritized.
Training and Competency
Healthcare providers involved in emergency care should be trained in transcutaneous pacing techniques. Competency in performing TCP is vital to ensure patient safety and effective treatment. Regular training and simulation exercises can enhance the skills necessary for successful pacing.
Conclusion
Transcutaneous pacing is a life-saving procedure that provides temporary cardiac support in emergencies involving bradycardia. Its non-invasive nature, ease of use, and effectiveness make it an invaluable tool in emergency medical settings. By understanding the indications, procedures, and potential complications associated with transcutaneous pacing, healthcare providers can deliver timely and effective care to patients experiencing severe cardiac events. As advancements in medical technology continue, transcutaneous pacing will remain a critical component of emergency cardiac management.