Celiac disease is a chronic autoimmune disorder where the ingestion of gluten—found in wheat, barley, and rye—triggers an immune response that damages the small intestine. This condition can cause a variety of symptoms and lead to long-term health issues if not properly managed. This article will explore the causes, symptoms, diagnosis, and management of celiac disease, offering a comprehensive guide for those affected and those seeking to understand it better.
What is Celiac Disease?
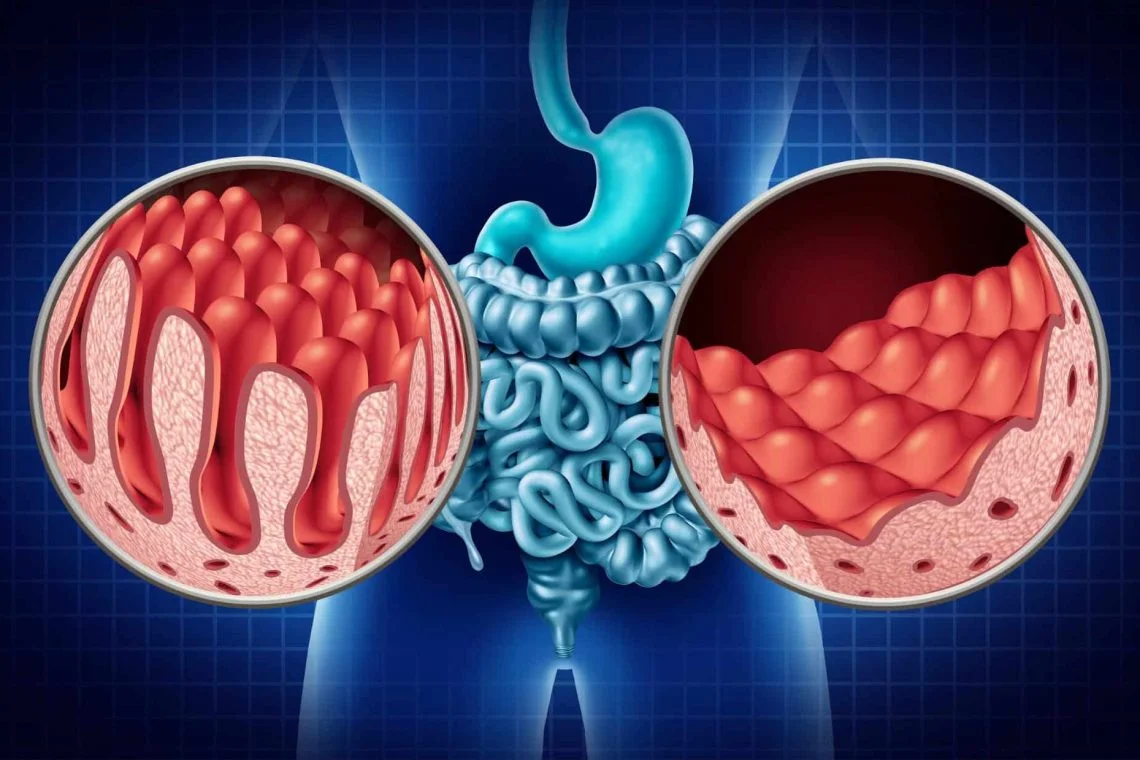
Celiac disease is an autoimmune disorder where the body’s immune system mistakenly targets the small intestine after consuming gluten, a protein found in wheat, barley, and rye. This immune reaction causes inflammation and damage to the villi, tiny hair-like structures in the small intestine that are essential for nutrient absorption. When these villi are damaged, the body is unable to absorb nutrients effectively, leading to a range of health issues.
The Role of Gluten
Gluten is a group of proteins found in certain grains. For most people, gluten is harmless, but in individuals with celiac disease, it triggers an autoimmune response. When someone with celiac disease consumes gluten, their immune system perceives it as a threat and attacks the lining of the small intestine.
Causes of Celiac Disease
Celiac disease is influenced by a combination of genetic and environmental factors.
Genetic Predisposition
Celiac disease has a strong genetic component. It is commonly associated with specific genes known as HLA-DQ2 and HLA-DQ8. Most people with celiac disease have one or both of these genetic markers, though having these genes does not guarantee that a person will develop the condition. Genetic testing can help determine if someone has a higher risk of celiac disease.
Environmental Factors
While genetics play a significant role, environmental factors are also important. These can include:
- Dietary Factors: Introducing gluten into the diet at a very young age, or not introducing it until later, may influence the development of celiac disease.
- Infections: Certain viral infections or gastrointestinal infections might trigger the onset of celiac disease in genetically predisposed individuals.
- Gut Health: The health of the gut microbiome may also play a role in the development of celiac disease. An imbalance in gut bacteria might contribute to the autoimmune response.

Symptoms of Celiac Disease
The symptoms of celiac disease can vary widely and may affect different parts of the body. They can range from mild to severe and may differ between adults and children.
Gastrointestinal Symptoms
The most common symptoms of celiac disease involve the digestive system:
- Diarrhea: Frequent, loose, and watery stools.
- Abdominal Pain: Cramping or discomfort in the abdomen.
- Bloating: Feeling of fullness or swelling in the abdomen.
- Gas: Increased flatulence.
- Constipation: Difficulty passing stools, less common but possible.
Non-Gastrointestinal Symptoms
Celiac disease can also present with symptoms not related to the digestive system:
- Fatigue: Persistent tiredness and lack of energy.
- Weight Loss: Unexplained weight loss despite normal or increased appetite.
- Anemia: Iron-deficiency anemia due to poor nutrient absorption.
- Skin Rash: Dermatitis herpetiformis, a blistering rash that usually appears on elbows, knees, and buttocks.
- Joint Pain: Aches or stiffness in the joints.
- Bone Disorders: Osteoporosis or osteopenia due to calcium and vitamin D malabsorption.
Symptoms in Children
In children, celiac disease may present differently:
- Delayed Growth: Poor growth or failure to thrive.
- Short Stature: Shorter than expected height.
- Behavioral Issues: Irritability or behavioral changes.
- Dental Enamel Defects: Abnormalities in the enamel of the teeth.
Diagnosing Celiac Disease
Diagnosing celiac disease involves a combination of medical history, blood tests, and sometimes a biopsy of the small intestine.
Blood Tests
Blood tests are often the first step in diagnosing celiac disease. These tests look for specific antibodies that are elevated in people with celiac disease. Common tests include:
- Tissue Transglutaminase Antibody Test (tTG-IgA): Measures antibodies against the enzyme tissue transglutaminase.
- Endomysial Antibody Test (EMA-IgA): Detects antibodies against the endomysium, a connective tissue in the body.
- Deamidated Gliadin Peptide (DGP) Test: Measures antibodies against gliadin, a component of gluten.
Biopsy
If blood tests suggest celiac disease, a small intestine biopsy is often performed to confirm the diagnosis. During this procedure, a small tissue sample is taken from the small intestine and examined for damage to the villi.
Genetic Testing
Genetic testing can also be useful in diagnosing celiac disease, particularly if blood tests and biopsy results are inconclusive. It can confirm the presence of the HLA-DQ2 or HLA-DQ8 genes associated with the condition.
Managing Celiac Disease
The primary treatment for celiac disease is a strict, lifelong gluten-free diet. This means avoiding all foods and products containing gluten. Managing celiac disease involves several steps:
Gluten-Free Diet
Following a gluten-free diet is crucial for managing celiac disease and preventing damage to the small intestine. This means eliminating foods like:
- Wheat: Includes all forms such as flour, semolina, and durum wheat.
- Barley: Found in malt, beer, and some cereals.
- Rye: Often used in bread and some baked goods.
- Oats: Must be certified gluten-free as they can be contaminated with gluten during processing.
Reading Labels
Carefully reading food labels is essential. Many processed foods contain hidden sources of gluten, so always check ingredient lists and look for products labeled “gluten-free.”
Avoiding Cross-Contamination
Cross-contamination can occur when gluten-free foods come into contact with gluten-containing products. To avoid this:
- Use Separate Utensils: For preparing gluten-free foods, use separate kitchen tools and surfaces.
- Be Cautious with Eating Out: Inform restaurant staff about your dietary needs and ask about their procedures to avoid cross-contamination.
Nutritional Considerations
A gluten-free diet can sometimes lack essential nutrients. It is important to:
- Consume a Balanced Diet: Ensure you get enough fiber, vitamins, and minerals from gluten-free sources.
- Consider Supplements: Consult with a healthcare provider about taking supplements if needed, especially for nutrients like iron, calcium, and vitamin D.
Living with Celiac Disease
Celiac disease requires ongoing management and lifestyle adjustments. Support from healthcare professionals, family, and support groups can be invaluable.
Emotional and Social Impact
Living with celiac disease can sometimes lead to emotional challenges, such as feelings of isolation or frustration. Connecting with others who have the condition through support groups or online communities can provide emotional support and practical advice.
Planning for Travel and Social Events
Traveling and attending social events can be challenging when managing celiac disease. Some tips include:
- Plan Ahead: Research restaurants and food options before traveling.
- Communicate: Inform hosts and restaurant staff about your dietary needs.
- Carry Snacks: Bring gluten-free snacks and meals to avoid limited options.
Regular Medical Follow-Up
Regular check-ups with a healthcare provider are important to monitor the health of the small intestine and ensure nutritional needs are met. Follow-up visits may include:
- Blood Tests: To check for any signs of ongoing inflammation or nutrient deficiencies.
- Bone Density Scans: To monitor bone health, particularly if osteoporosis is a concern.
Research and Advances
Research into celiac disease is ongoing, and new treatments and diagnostic methods are continually being developed. Some areas of interest include:
- Vaccine Development: Researchers are exploring vaccines that could help the immune system tolerate gluten.
- Enzyme Therapy: Investigating enzymes that might break down gluten in the digestive system before it triggers an immune response.
- Alternative Therapies: Studying other potential treatments and interventions to help manage or mitigate symptoms.
Conclusion
Celiac disease is a serious autoimmune condition that requires lifelong management through a strict gluten-free diet. Understanding the causes, recognizing the symptoms, and following appropriate diagnostic and treatment measures are crucial for effectively managing this condition. With careful planning and support, individuals with celiac disease can lead healthy and fulfilling lives.
For anyone experiencing symptoms or who has been diagnosed with celiac disease, consulting with a healthcare provider for personalized advice and treatment is essential. Through continued research and advances in the field, the outlook for managing celiac disease continues to improve, offering hope for better treatments and a more comprehensive understanding of this complex condition.