Introduction
Hyperkalemia is a medical condition characterized by elevated levels of potassium in the blood. Potassium is an essential electrolyte that plays a vital role in various bodily functions, including muscle contractions and heart rhythm regulation. When potassium levels become too high, it can lead to serious complications, particularly affecting the heart. One of the most critical tools for diagnosing and monitoring hyperkalemia is the EKG (electrocardiogram). In this article, we will explore what hyperkalemia is, how it affects the heart, and the significance of the hyperkalemia EKG in clinical practice.
What is Hyperkalemia?
Hyperkalemia is defined as a serum potassium level greater than 5.0 mmol/L. Potassium is crucial for maintaining normal cellular function, particularly in nerve and muscle cells. The kidneys typically regulate potassium levels, excreting excess amounts to maintain homeostasis. However, several factors can disrupt this balance, leading to hyperkalemia.
Causes of Hyperkalemia
There are several causes of hyperkalemia, including:
- Renal Failure: The most common cause, where the kidneys cannot excrete potassium effectively.
- Medications: Certain drugs, such as ACE inhibitors, potassium-sparing diuretics, and nonsteroidal anti-inflammatory drugs (NSAIDs), can increase potassium levels.
- Tissue Breakdown: Conditions like rhabdomyolysis or hemolysis can release potassium into the bloodstream.
- Acidosis: Conditions that cause metabolic acidosis can shift potassium from inside cells to the extracellular fluid.
- Dietary Intake: Excessive consumption of potassium-rich foods or supplements can also contribute.
Symptoms of Hyperkalemia
Mild hyperkalemia may not cause noticeable symptoms, but as potassium levels rise, patients may experience:
- Fatigue
- Weakness
- Nausea
- Palpitations
- Muscle cramps
- Cardiac arrest in severe cases
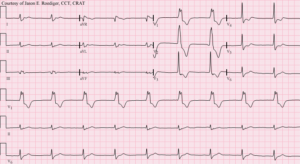
The Role of EKG in Hyperkalemia
An EKG is a diagnostic tool that measures the electrical activity of the heart. It provides essential information about the heart’s rhythm and can help identify abnormalities that may indicate hyperkalemia.
How Hyperkalemia Affects EKG Readings
High potassium levels have a significant impact on the heart’s electrical conduction system, leading to characteristic changes on an EKG. These changes can be classified into several stages, which we will explore in detail.
Stage 1: Peaked T Waves
The first noticeable change in a hyperkalemia EKG is the appearance of tall, peaked T waves. These T waves are typically symmetrical and can be seen in the precordial leads (V2 to V6).
- Mechanism: Elevated potassium levels lead to increased myocardial excitability, which causes the repolarization phase to become altered, resulting in peaked T waves.
Stage 2: Prolonged PR Interval
As potassium levels continue to rise, the PR interval on the EKG may become prolonged. The PR interval represents the time taken for the electrical impulse to travel from the atria to the ventricles.
- Mechanism: High potassium levels can affect the conduction through the atrioventricular (AV) node, leading to delays in impulse transmission.
Stage 3: Widened QRS Complex
With further increases in potassium levels, the QRS complex may become widened. The QRS complex represents the depolarization of the ventricles.
- Mechanism: The effects of high potassium on ventricular conduction lead to slower impulse propagation through the ventricles, resulting in a wider QRS complex.
Stage 4: Loss of P Waves
As hyperkalemia progresses, P waves may become difficult to identify or may completely disappear from the EKG.
- Mechanism: The increased potassium levels disrupt atrial depolarization, leading to the loss of P waves.
Stage 5: Sine Wave Pattern and Ventricular Fibrillation
In severe cases of hyperkalemia, a sine wave pattern may develop on the EKG, characterized by a merging of the QRS complex and T wave.
- Mechanism: This pattern indicates a critical state of hyperkalemia, which can lead to life-threatening arrhythmias, including ventricular fibrillation.
Importance of Early Detection
Recognizing these EKG changes is crucial for the timely management of hyperkalemia. Early detection and treatment can prevent severe complications, such as cardiac arrest.
Diagnosing Hyperkalemia
Laboratory Tests
Diagnosis of hyperkalemia typically begins with a blood test to measure serum potassium levels.
- Normal Range: A normal serum potassium level is between 3.5 and 5.0 mmol/L.
- Critical Levels: Levels above 6.0 mmol/L are considered critical and require immediate intervention.
EKG Monitoring
In patients with suspected hyperkalemia, continuous EKG monitoring is essential. Changes on the EKG can provide real-time information about the patient’s cardiac status and the severity of hyperkalemia.
Management of Hyperkalemia
Immediate Treatment
If hyperkalemia is diagnosed, immediate treatment options may include:
- Calcium Administration: Calcium gluconate or calcium chloride can stabilize the cardiac membrane and protect the heart from the effects of high potassium levels.
- Insulin and Glucose: Administering insulin along with glucose helps to drive potassium back into the cells, temporarily lowering serum potassium levels.
- Beta-agonists: Medications like albuterol can also help shift potassium intracellularly.
- Sodium Bicarbonate: In cases of metabolic acidosis, sodium bicarbonate can be administered to help restore acid-base balance and shift potassium into cells.
- Diuretics: Loop diuretics can promote renal excretion of potassium in patients with adequate kidney function.
- Dialysis: In severe cases or when other treatments are ineffective, dialysis may be necessary to remove excess potassium from the blood.
Long-term Management
Managing the underlying cause of hyperkalemia is crucial for preventing recurrence. This may involve:
- Adjusting Medications: Reviewing and potentially discontinuing medications that contribute to hyperkalemia.
- Dietary Modifications: Educating patients about foods high in potassium and creating a balanced diet plan.
- Monitoring Kidney Function: Regular follow-ups with blood tests to monitor kidney function and potassium levels.
Conclusion
Hyperkalemia is a potentially life-threatening condition that can significantly impact heart function. Understanding the relationship between hyperkalemia and EKG changes is essential for timely diagnosis and treatment. The hyperkalemia EKG reveals distinct patterns that can indicate rising potassium levels, allowing for prompt intervention.
Regular monitoring and appropriate management strategies are crucial for patients at risk of hyperkalemia. By staying informed about the causes, symptoms, and EKG changes associated with hyperkalemia, healthcare providers can improve patient outcomes and prevent serious complications.
In summary, recognizing the signs of hyperkalemia on an EKG can save lives, and understanding this relationship is essential for both healthcare professionals and patients alike.
Additional Information
Lifestyle Modifications
In addition to medical management, certain lifestyle changes can help manage potassium levels effectively:
- Diet: Reducing the intake of potassium-rich foods such as bananas, oranges, tomatoes, potatoes, and spinach can be beneficial for patients at risk.
- Hydration: Maintaining adequate fluid intake is important for kidney function and potassium excretion.
- Regular Exercise: Engaging in regular physical activity can help maintain overall health and improve cardiovascular function.
- Education: Patients should be educated about the signs and symptoms of hyperkalemia and the importance of adhering to treatment plans.
Future Directions in Hyperkalemia Management
Research continues to evolve in the understanding and management of hyperkalemia. New treatments and medications are being developed to provide better control of potassium levels, especially in patients with chronic kidney disease or heart failure.
- New Drugs: Medications that promote potassium excretion while being safe for patients with heart or kidney conditions are under investigation.
- Personalized Treatment: Future management strategies may focus on personalized approaches based on individual patient profiles, including genetic factors affecting potassium metabolism.
Conclusion
In conclusion, hyperkalemia is a serious condition that requires attention and understanding. The hyperkalemia EKG serves as a vital tool in diagnosing and managing this electrolyte imbalance. By recognizing the changes in EKG patterns, healthcare professionals can take swift action to mitigate the risks associated with high potassium levels. Through a combination of immediate treatment, lifestyle modifications, and ongoing research, the future of hyperkalemia management looks promising. Staying informed and proactive in managing potassium levels can lead to better health outcomes and a higher quality of life for those affected by this condition.